The ability to connect specific clinical challenges with focused academic innovation can be critical to the development of products that will deliver tangible patient impact. This is particularly true for medical devices, as with our revolutionary eye-drop to prevent corneal scarring and blindness.
 What: Revolutionary eye-drop to prevent corneal scarring and blindness
What: Revolutionary eye-drop to prevent corneal scarring and blindness
Why: Injuries to the surface of the eye are a leading cause of visual loss, but there are few therapeutic options to modify, minimise or reverse scarring
How: Birmingham hosts the largest medical device cluster in the UK with an impressive and extensive infrastructure in addition to world class hospital trusts
Injuries to the surface of the eye as a result of burns, infections, inflammation, trauma and surgery, can cause corneal scarring and opacity – a leading cause of visual loss. There are few therapeutic options to modify, minimise or reverse scarring to maintain corneal transparency and visual function, and these are not always effective. With a global prevalence of 5.1%, the incidence of visual loss is ~8 million people/year and costs ~£150 billion/year, and the WHO has consequently made this a priority area programme to prevent world-wide blindness.
Birmingham hosts the largest medical device cluster in the UK with an impressive and extensive infrastructure in addition to world class hospital trusts, including the Institute for Translational Medicine and the new Medical Device Testing and Evaluation Centre (MD-TEC) linked to our Healthcare Technology Research Institute. Co-located with a host of clinical/academic centres of excellence focused on translational challenges – such as the NIHR Surgical Reconstruction and Microbiology Research Centre (SRMRC) – this provides academics, clinicians and industry with a perfect environment to rapidly mature their nascent technologies, provide training opportunities, and act as an integrated coordination point to bring multi-disciplinary teams together around shared challenges and opportunities.
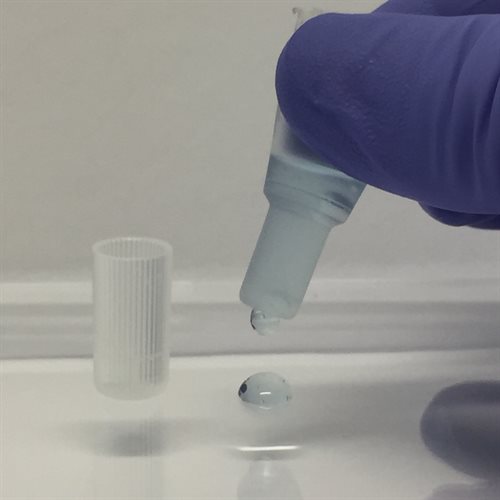
In this case, bringing together neurosciences and ophthalmology expertise with Professor Liam Grover’s healthcare technologies team led to the discovery that combining decorin and collagen results in enhanced anti-scarring bioactivities, creating a microenvironment that enables anti-fibrotic and anti-inflammatory factors to promote scarless wound healing and improve clinician and/or patient-reported visual outcomes. The combination of academic, clinical and technological expertise we were able to bring together rapidly pushed this along a translational escalator – securing over £5million through internal and external funding schemes from MRC, Wellcome Trust and NIHR to accelerate development of a synthetic, transparent, anti-scarring eye drop for the management of patients at risk of corneal scarring.
 In 2018 we will lead the first in-human clinical trial to assess the treatment’s safety and efficacy in patients with microbial keratitis. This will create a unique collaboration between the University of Birmingham, Birmingham and Midland Eye Centre, Sandwell and West Birmingham Hospitals NHS Trust and the Queen Elizabeth Hospital Birmingham. The clinical trial will also help move the technology along the translational pathway towards regulatory approvals and commercial realisation. The research team has already consulted with patients, practitioners and regulatory bodies, and potential commercial partners have also registered their interest in the technology.
In 2018 we will lead the first in-human clinical trial to assess the treatment’s safety and efficacy in patients with microbial keratitis. This will create a unique collaboration between the University of Birmingham, Birmingham and Midland Eye Centre, Sandwell and West Birmingham Hospitals NHS Trust and the Queen Elizabeth Hospital Birmingham. The clinical trial will also help move the technology along the translational pathway towards regulatory approvals and commercial realisation. The research team has already consulted with patients, practitioners and regulatory bodies, and potential commercial partners have also registered their interest in the technology.
The anti-scarring eye drop will not only have significant positive impacts for patients, but also socio-economic impacts – patients with ocular damage will carry a reduced direct and indirect cost of treatment burden as the eye drop may be self-administered in a home and/or community setting, negating the need for prolonged hospitalisation and clinic attendance. In the not too distant future, patients will be able to access this revolutionary sight-saving eye drop to prevent the devastating consequences of corneal damage.