Inflammatory Mechanisms in the Ocular Environment
1) Ocular surface, scarring, regeneration and biomaterials
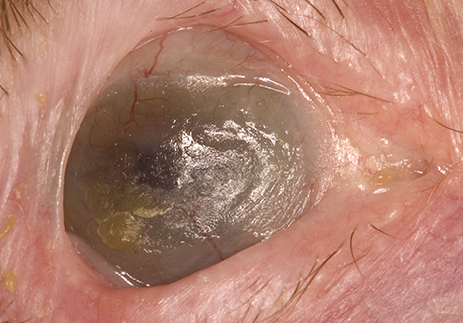
Inflammation and scarring of the ocular surface may occur secondary to trauma, iatrogenic (Stevens-Johnson Syndrome), or immune-mediated disease, such as Mucous Membrane Pemphigoid and Sjögren’s Syndrome. Persistent inflammation of the ocular surface leads to fibrosis, contracture of the conjunctiva, and in more severe cases may lead to ulceration, stem cell failure, corneal scarring and sight loss.
 We have described ongoing conjunctival inflammation at a molecular level in the absence of clinically detectable inflammation using a novel technique of ocular surface impression cytology with flow cytometry (OSIC-flow) (Miss Rauz and Dr Curnow) and applied this to diseases such as SJS/TEN, MMP, GVHD and Sjögren’s Syndrome. Corneal scarring is a leading cause of blindness worldwide and forms a WHO priority area for development of new therapies to prevent blindness. The Neurotrauma Research Group (Prof Logan) and Chemical Engineering (Prof Grover) are working closely with the Academic Unit of Ophthalmology (Miss Rauz) and the Department of Pharmacology (Prof Barnes) at the University of Birmingham to develop a highly innovative and revolutionary fluid-gel technology that enables a microenvironment with anti-fibrotic and anti-inflammatory factors that promote scarless wound healing. The research collaboration is a recipient of the highly prestigious Major Direct Pathway Finding Scheme Medical Research Council (MRC) Award to develop a sight-saving synthetic, optically-transparent, anti-scarring dressing for the prevention of corneal scarring.
We have described ongoing conjunctival inflammation at a molecular level in the absence of clinically detectable inflammation using a novel technique of ocular surface impression cytology with flow cytometry (OSIC-flow) (Miss Rauz and Dr Curnow) and applied this to diseases such as SJS/TEN, MMP, GVHD and Sjögren’s Syndrome. Corneal scarring is a leading cause of blindness worldwide and forms a WHO priority area for development of new therapies to prevent blindness. The Neurotrauma Research Group (Prof Logan) and Chemical Engineering (Prof Grover) are working closely with the Academic Unit of Ophthalmology (Miss Rauz) and the Department of Pharmacology (Prof Barnes) at the University of Birmingham to develop a highly innovative and revolutionary fluid-gel technology that enables a microenvironment with anti-fibrotic and anti-inflammatory factors that promote scarless wound healing. The research collaboration is a recipient of the highly prestigious Major Direct Pathway Finding Scheme Medical Research Council (MRC) Award to develop a sight-saving synthetic, optically-transparent, anti-scarring dressing for the prevention of corneal scarring.
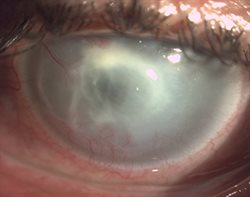
Disruption of ocular defence mechanisms following contact-lens wear, corneal trauma, herpes simplex virus, corneal anaesthesia, corneal exposure, and ocular surface disease predisposes the eye to severe corneal infection known as microbial keratitis, one of the commonest causes of worldwide blindness. The Academic Unit of Ophthalmology (Miss Rauz), NIHR Surgical Reconstruction and Microbiology Research Centre and the School of Biosciences (Dr Loman) are developing a novel non-culture technique for the molecular diagnosis of microbial keratitis using whole genome sequencing.
2) Uveitis
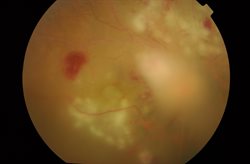
The eye is made up of three main layers, an outer tough coating (sclera), a middle layer (uvea) and an inner light-sensing layer (retina). Inflammation of the uvea is known as uveitis.
 Studies conducted by the Academic Unit of Ophthalmology (Prof PI Murray and Dr Wallace) have shown that the inflammatory process in uveitis consists of a complex interplay of host genetics, immune cells (macrophage, neutrophils, dendritic cells, T-cells), their signalling molecules (cytokines, i.e. IL-6), and environment (medications to dampen the immune system). The cause of most uveitis cases is unknown and there is no reliable diagnostic test. In collaboration with the National Institutes of Health (NIH), Bethesda, USA, Dr Wallace is developing a novel machine learning method known as the ‘supercell analysis’ to identify the differences in the blood cells of patients with uveitis and healthy volunteers which could lead to a reliable diagnostic test in the future.
Studies conducted by the Academic Unit of Ophthalmology (Prof PI Murray and Dr Wallace) have shown that the inflammatory process in uveitis consists of a complex interplay of host genetics, immune cells (macrophage, neutrophils, dendritic cells, T-cells), their signalling molecules (cytokines, i.e. IL-6), and environment (medications to dampen the immune system). The cause of most uveitis cases is unknown and there is no reliable diagnostic test. In collaboration with the National Institutes of Health (NIH), Bethesda, USA, Dr Wallace is developing a novel machine learning method known as the ‘supercell analysis’ to identify the differences in the blood cells of patients with uveitis and healthy volunteers which could lead to a reliable diagnostic test in the future.
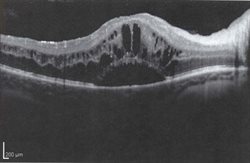 The Academic Unit of Ophthalmology (Prof PI Murray) is actively involved in undertaking Pharmaceutical clinical trials for new therapies for uveitis. At present this involves looking at a long acting steroid pellet that is injected into the eye funded by the Medical Research Council and National Institute for Health Research comparing two biological drugs (alpha interferon and infliximab) for the treatment of Behçet’s Disease. Developing novel imaging techniques using Optical Coherence Tomography as a validated methodology to accurately quantify inflammation inside the eye that could be used in the clinic and in drug trials forms a focus (Prof Murray, Mr Denniston). The work has recently expanded in to more qualitative research exploring the quality of life issues that uveitis patients who have poor central vision related to their inflammation (cystoid macular oedema) experience. This would lead to the development of a Core Outcome Set of Patient Report Outcomes that could be added to the outcomes already measured in clinical trials of new drugs.
The Academic Unit of Ophthalmology (Prof PI Murray) is actively involved in undertaking Pharmaceutical clinical trials for new therapies for uveitis. At present this involves looking at a long acting steroid pellet that is injected into the eye funded by the Medical Research Council and National Institute for Health Research comparing two biological drugs (alpha interferon and infliximab) for the treatment of Behçet’s Disease. Developing novel imaging techniques using Optical Coherence Tomography as a validated methodology to accurately quantify inflammation inside the eye that could be used in the clinic and in drug trials forms a focus (Prof Murray, Mr Denniston). The work has recently expanded in to more qualitative research exploring the quality of life issues that uveitis patients who have poor central vision related to their inflammation (cystoid macular oedema) experience. This would lead to the development of a Core Outcome Set of Patient Report Outcomes that could be added to the outcomes already measured in clinical trials of new drugs.
3) Infections, immunity and Microbiome
 The gut microbiome is important in the development and maintenance of a healthy immune system. Changes in the gut microbiome are linked to the body’s immune system misbehaving and leading to various diseases, such as inflammatory bowel disease and rheumatoid arthritis. In collaboration with Nick Loman (School of Biosciences) the group (Miss Rauz, Dr Wallace, Prof Murray) are evaluating the potential role of the gut microbiome as a driver of inflammation in inflammatory eye disease in genetically predisposed individuals, and whether gut microbiome changes with systemic treatment to dampen the immune system.
The gut microbiome is important in the development and maintenance of a healthy immune system. Changes in the gut microbiome are linked to the body’s immune system misbehaving and leading to various diseases, such as inflammatory bowel disease and rheumatoid arthritis. In collaboration with Nick Loman (School of Biosciences) the group (Miss Rauz, Dr Wallace, Prof Murray) are evaluating the potential role of the gut microbiome as a driver of inflammation in inflammatory eye disease in genetically predisposed individuals, and whether gut microbiome changes with systemic treatment to dampen the immune system.