Blocking cancer's ability to switch off the immune response can unleash powerful anti-tumour effects, reports Luke Harrison.
It has been said that even the least intelligent cancer can outsmart the most intelligent scientist. But research being carried out at the University of Birmingham suggests that a change is on the horizon; and that cancer’s time on top might be coming to an end.
Director of the University’s Cancer Immunology and Immunotherapy Centre Professor Ben Willcox would certainly agree.
‘Research into cancer immunology has come a long way in the last two or three years; there have been significant strides within the field towards understanding the mechanisms within individual tumours. Perhaps the best way to explain it is to compare it to being a mechanic getting under the bonnet of a car and getting to grips with the valves and pistons for the first time.’
The wealth of garnered knowledge into the inner-workings of the tumour has given rise to new possibilities in countering the two biggest challenges; what to target in the tumour, and how to then effectively attack the cancerous cells.
Currently there is a dearth of individual targets deemed safe which limits the range of therapies available, so a key focus of the work at Birmingham is to understand what we are able to target within specific tumours.
Professor Willcox explains, ‘There are some really interesting tumour-specific targets emerging from research groups at Birmingham. My own research focuses on an unconventional set of immune cells, gamma delta T-cells, which have, evolutionarily speaking, existed for a long time – but we don’t really understand them. We understand that they can kill cancer cells, so they’re very interesting therapeutically, and we are trying to understand what they are recognising, and how to harness that power to treat patients.’
Of course, knowing your enemy is complicated, particularly with an adversary as diverse and crafty as cancer. Even if we take care of the ‘what’, the ‘how’ could be much more complicated.
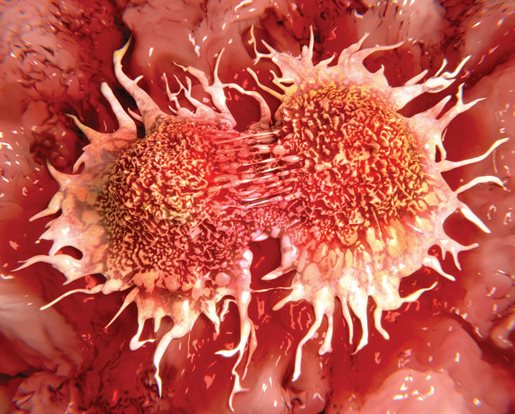
Although cancerous cells can generate a strong immune response against them, in many cases they’re highly capable of turning the response off.
But groundbreaking advances, particularly from research in the US, have shown that by stopping the ability of tumours to hit the ‘off switch’ on the immune response it is possible to unleash powerful anti-tumour effects.
‘We’ve already seen an impact on patient treatment where people even in the latter stages of cancer may actually be starting to see a turnaround. Removing the brakes on the immune response is a great starting point but now it’s a case of giving those immune cells the boost they need to be as effective as possible when they reach the target cells.
‘The immune system is finely balanced on a tightrope between being strong enough to defend against infection but not so strong that it attacks your own body. So any engineering or boosting of these immune cells, ‘pimping them up’ as it were, needs to be both effective and smart.’
The future of cancer immunology hinges on how these sets of knowledge are used. ‘It becomes almost like molecular Lego. How can we add this to this antibody? How can we attach bits on to make it a more powerful way of targeting tumours? And how do we make sure that we’re using the right pieces for the right tumour in the right patients?
‘It’s reaching a point where the creativity of the scientists comes into play, and part of the reason Birmingham has a big role to play in this area is because we have some very creative scientists.’
The University also benefits from having a wealth of local resources; the academic rigour of the Cancer Immunology and Immunotherapy Centre, one of Europe’s largest Clinical Trials Units and the proximity to University Hospitals Birmingham.
‘We’re going to learn a lot directly from patients in developing new therapies. Not all patients are the same and actually we need to, in a sense, listen to the tumour to understand what the individual profile of a tumour is like, what’s going on under this particular bonnet?’
The team at Birmingham is working to develop stratified treatments for different patient groups; allowing clinicians to assess, in a useable clinical framework and timeframe, which group a particular patient falls into and what therapy they need to get.
Professor Willcox takes particular pride in noting how fundamental research from our labs can be tracked through to novel clinical trials that could have a major impact on patient treatment.
‘Seeing new therapies in development, therapies that have been born from Birmingham research into the nuts and bolts of cancer immunology, gives us great hope. The advances we are making here, including understanding how to gear them towards individual patients, appear to have put us firmly in the driving seat.’