The autoimmune disorder of the nervous system linked to an underlying tumour is due to an attempt by the immune system to subjugate the growth of the tumour expressing neuronal antigens. The unfortunate consequence of this results in a rapid onset of neurological deficits known as Paraneoplastic Neurological Syndrome (PNS). This phenomenon is rare (<1%) and often accompanied by specific high-titre autoantibodies which are non-pathogenic, react with intracellular antigens and represents T-cell mediated response. These are very useful early diagnostic markers of PNS and also, in some cases, underlying malignancy thus facilitating faster diagnosis and earlier treatment with better prognosis.
Management of PNS
Treatment of the paraneoplastic neurological syndrome is primarily the identification and treatment of the underlying tumour. However, in many patients a trial of immunotherapy may be necessary and this can be effective in most syndromes, especially after the appropriate treatment for the tumour.
Summary of paraneoplastic neurological antibodies
| Antibody | Staining pattern | PND | Associated tumours |
|---|
| Recoverin |
Retinal photoreceptor |
CAR |
SCLC, thymoma |
| Yo (PCA-1) |
Purkinje cell cytoplasm & axons |
PCD |
Ovarian, breast |
| Ma (Ma1) |
Neuronal nucleoli of the neuronal cells |
PCD, BE |
Various cancer |
| Ta (Ma2) |
Neuronal nucleoli of the neuronal cells |
PCD, LE |
Testicular cancer |
| Hu (ANNA1) |
Nuclei of both central and peripheral neurones |
PCD, PEM, SN |
SCLC |
| Ri (ANNA2) |
Nuclei of central neurones |
OM, PCD, BE |
Breast, SCLC, gynaecological |
| GAD |
Islet cells & grey matter |
SPS |
Breast, colon, SCLC |
| CV2/CRMP5 |
Oligodendrocytes cytoplasm |
PEM, SN |
SCLC, thymoma |
| Amphiphysin |
Central presynaptic terminals |
SPS, SN |
Breast cancer, SCLC |
| mGluR1 |
Purkinje cell cytoplasm, climbing fibre |
PCD |
Hodgkin’s lymphoma |
| ANNA-3 |
Purkinje cell cytoplasm & nucleus + glomerular podocytes |
PCD, PEM, SN |
SCLC |
| PCA-2 |
Purkinje cell cytoplasm and other neurones |
PEM, PCD, LEMS |
SCLC |
| SOX1 (AGNA) |
Nuclei of Bergmann glia of cerebellar Purkinje layer and glial in white matter |
PND |
SCLC |
| Zic4 |
Staining seen in the neuronal nuclei of cerebellar granular layer (but not Purkinje cells) |
PCD |
SCLC |
| PCA-Tr |
Purkinje cell cytoplasm with “dots” in molecular layer |
PCD |
Hodgkin’s lymphoma |
| Titin |
Stains striations in the skeletal muscle |
MG |
Thymoma |
KEY: PND = paraneoplastic neurological disorder, PCD = paraneoplastic cerebellar degeneration, PEM = paraneoplastic encephalomyelitis, SN = sensory neuropathy, OM= opsoclonus/myclonus, BE = brainstem encephalomyelitis, LE = limbic encephalomyelitis, LEMS = Lambert-Eaton myasthenic syndrome, SPS = Stiff person syndrome, CAR = Cancer Associated Retinopathy. MG = Myasthenia Gravis, SCLC= small cell lung carcinoma, AGNA = anti-glial nuclear antibody, DNER = Delta/Notch-like Epidermal Growth Factor-Related Receptor, SOX1 = gene that encodes a transcription factor with a HMG-box.
Cerebellar architecture
Paraneoplastic neurological antibodies: For detection of these, it is necessary to be familiar with cerebellar histology.
The cerebellum consists of the white and the grey matter. The latter is subdivided into Molecular, Purkinje cell and Granular layer (contains densely packed granular cells). The Purkinje cells can easily be identified due their large size. These are located on the border of granular and molecular layer.
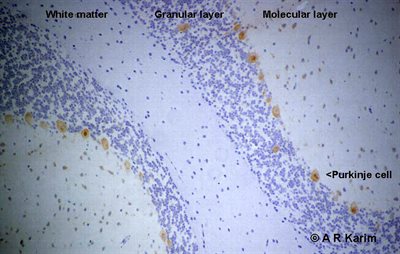 The most favoured method for detection of paraneoplastic antibodies is to screen patient’s serum on cerebellum and any positive reaction producing identifiable pattern is further confirmed by alternative method such as line blot consisting painted recombinant proteins.
The most favoured method for detection of paraneoplastic antibodies is to screen patient’s serum on cerebellum and any positive reaction producing identifiable pattern is further confirmed by alternative method such as line blot consisting painted recombinant proteins.